Welcome to this article on health economic evaluation. We will have a very broad look at what it is and introduce the four main types of economic evaluations. So, first of all, why do we need health economic evaluations?
There are many effective and worthwhile health interventions or programs that can improve the health of a population. If we had a lot of money to spend, we could use it for every beneficial health program.
The reality, however, is that we usually don't. If we spend all the money on one intervention, we don't have any left for others. This is called an opportunity cost. Because of this, difficult decisions have to be made to ensure a limited amount of money is spent to achieve the most benefit.
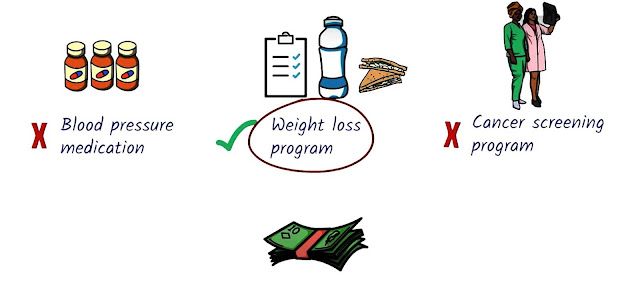
Health economic evaluation is a tool that helps with making those decisions. It allows us to compare two or more health interventions based on their costs and outcomes.
Four main types of economic evaluations
- cost minimization;
- cost-effectiveness;
- cost-utility;
- cost-benefit analysis.
They all compare costs with the outcome but do so in different ways. Direct costs are costs that are directly associated with an intervention. For example, the cost of medicines equipment like X-ray machines, salaries of healthcare staff, or the cost of transport to the health centre.
Direct costs are the main focus of most economic evaluations. Indirect costs are, costs associated with reduced productivity due to the illness or its treatment. An example is missed wages because of not working due to the illness.
Intangible costs are subjective, such as pain, suffering or grief due to the illness or treatment. These costs are quite hard to put a monetary value on that's. A look at the Different Types of Costs.
Different types of economic evaluations
Cost minimization analysis
This type of analysis used when the product or outcome is the same and what we're comparing is the cost. For example. We're comparing blood pressure reducing medications made by different manufacturers and have different prices. In a cost-minimization analysis, we simply compare the costs because the medicine is the same.
Cost-effectiveness analysis
This is used when we're comparing different interventions that have a common health outcome. Examples of health outcomes are reduction in blood pressure, cancer cases avoided, kilos lost, or life-years gained. These are called natural units.
Let's take a look at an example. We're comparing two interventions to reduce weight, a diet program and weight loss medication. The health outcome we're interested in is how many kilos have been lost. The diet program had a two-kilogram weight loss and cost $300. So the cost per kilo lost is $150. This is called a cost-effectiveness ratio.
Let's compare this with a medication based program that leads to a weight loss of 3 kg but costs $500. In this intervention, the cost per kilo lost is $500. So in this scenario, the diet based program is more cost-effective compared to the medication based program.
So a cost-effective analysis compares the cost per natural unit for different interventions. But what do we do if we want to compare interventions with different health outcomes? For this, we use a type of economic analysis called cost-utility analysis.
Cost-utility analysis
We want to compare drug therapy to reduce high blood pressure, breast screening to reduce the number of breast cancer cases, and a kidney transplant for end stage kidney disease to improve kidney function. These are different health interventions that have different health outcomes. So in order to compare these different interventions, we need to have a common outcome measure that can be applied to all these interventions. The measure that is most commonly used is called the Quality Adjusted Life Year (QALY).
What is a Quality Adjusted Life Year (QALY)
Health interventions try to prolong a person's life by increasing the number of years a person lives, and they also try to improve the quality of those years lived. A Quality Adjusted Life Year is a combined measure that considers both of these aspects.
A QALY is calculated by taking the number of extra years gained from the intervention and multiplying it by the quality of life of those extra years.
Quality of life is graded from zero to one, from zero being the worst possible health state and one being the best possible health state. There are many different ways to determine these gratings. They usually involve asking people how they rate their quality of life. A variety of tools can be used for this. Measures such as qualities are called health utility measures because they measure an individual's preference for different health outcomes.
Let's have a look at an example. If an intervention leads to a person living five years in perfect health, a health utility of one, then the number of QALY is gained as a result of this intervention is five.
Similarly, if an intervention leads to a person living an extra five years but with a quality of life of 0.2, then the QALY is gained as a result of that intervention is one. Now that we have a common outcome measure, a QALY. We can compare the cost per QALY across different interventions.
So a cost-utility analysis compares the cost of a utility measures such as a quality for different interventions.
Cost-benefit analysis
This type of analysis measures both the cost and outcome in monetary terms. A cost-benefit analysis tries to account for all costs and all benefits, direct, indirect, and intangible. To calculate benefits, a variety of tools can be used. The willingness to pay method determines the value that people attach to health outcomes.
For example, by asking people how much they're willing to pay to have the benefits of the treatment or to avoid the costs of illness. The human capital method places a monetary value on the person's life. The value is based on the loss or gain of income due to the illness. Although this type of evaluation is comprehensive, the data requirements can be quite high, and there are methodological issues when it comes to determining a value on life and productivity.
In reality, economic evaluations can be quite complex to do. Require various statistical calculations and adjustments such as stratification to adjust for different patient groups that might benefit differently from the interventions. Discounting to account for cost and benefits that occur at different times and sensitivity analysis to adjust for uncertainties in the data. That's a very quick introduction to health economic evaluation an important tool that helps us make decisions about allocating health resources.





Comments
Post a Comment